Hip fracture
A hip fracture is a serious injury, with complications that can be life-threatening. The risk of hip fracture rises with age.
Older people are at a higher risk of hip fracture because bones tend to weaken with age (osteoporosis). Multiple medications, poor vision and balance problems also make older people more likely to trip and fall — one of the most common causes of hip fracture.
A hip fracture almost always requires surgical repair or replacement, followed by months of physical therapy. Taking steps to maintain bone density and avoid falls can help prevent hip fracture.
Symptoms
Signs and symptoms of a hip fracture include:
- Inability to move immediately after a fall
- Severe pain in your hip or groin
- Inability to put weight on your leg on the side of your injured hip
- Stiffness, bruising and swelling in and around your hip area
- Shorter leg on the side of your injured hip
- Turning outward of your leg on the side of your injured hip
Causes
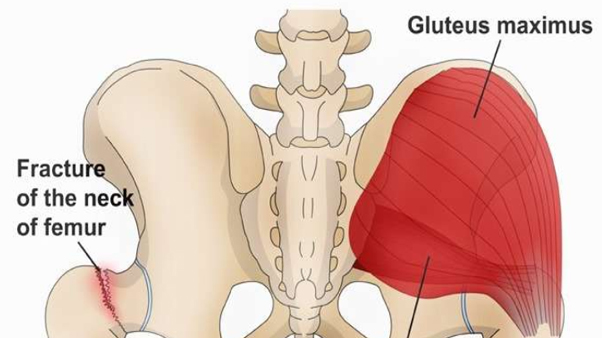
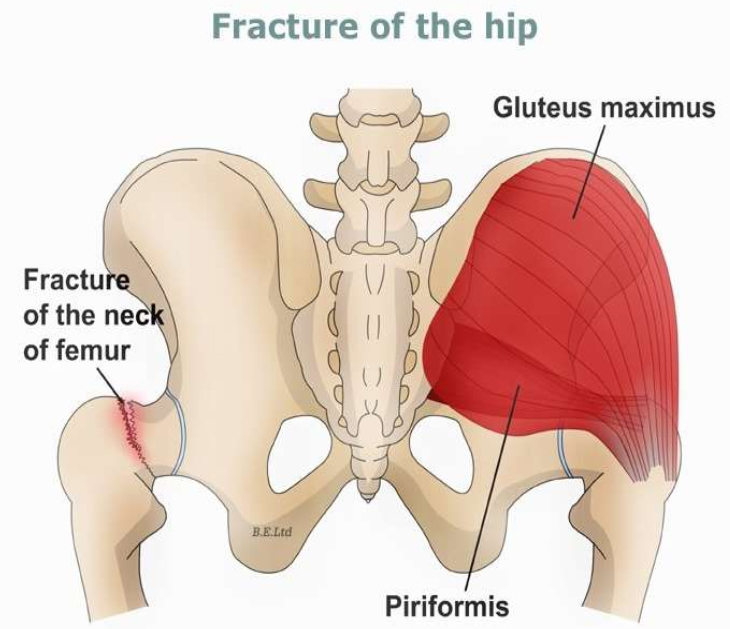
A severe impact — in a car crash, for example — can cause hip fractures in people of all ages. In older adults, a hip fracture is most often a result of a fall from a standing height. In people with very weak bones, a hip fracture can occur simply by standing on the leg and twisting.
Treatments and drugs
Treatment for hip fracture usually involves a combination of surgery, rehabilitation and medication.
Surgery
The type of surgery you have generally depends on the location and severity of the fracture, whether the broken bones aren’t properly aligned (displaced fracture), and your age and underlying health conditions. The options include:
- Internal repair using screws. Metal screws are inserted into the bone to hold it together while the fracture heals. Sometimes screws are attached to a metal plate that runs down the femur.
- Partial hip replacement. If the ends of the broken bone are displaced or damaged, your surgeon may remove the head and neck of the femur and install a metal replacement (prosthesis).
- Total hip replacement. Your upper femur and the socket in your pelvic bone are replaced with prostheses. Total hip replacement may be a good option if arthritis or a prior injury has damaged your joint, affecting its function even before the fracture.
Your doctor may recommend partial or total hip replacement if the blood supply to the ball part of your hip joint was damaged during the fracture. That type of injury, which occurs most often in older people with femoral neck fractures, means the bone is less likely to heal properly.
Rehabilitation
Your care team will probably get you out of bed and moving on the first day after surgery. Physical therapy will initially focus on range of motion and strengthening exercises. Depending on the type of surgery you had and whether you have assistance at home, you may need to go from the hospital to an extended care facility.
In extended care and at home, you may work with an occupational therapist to learn techniques for independence in daily life, such as using the toilet, bathing, dressing and cooking. Your occupational therapist will determine if a walker or wheelchair may help you regain mobility and independence.
Medication
About 20 percent of people who have a hip fracture will have another hip fracture within two years. Bisphosphonates may help reduce the risk of a second hip fracture.
Most of these drugs are taken orally and are associated with side effects that may be difficult to tolerate, including acid reflux and inflammation of the esophagus. To avoid these side effects, your doctor may recommend taking bisphosphonate via intravenous (IV) tubing.
Bisphosphonates generally aren’t recommended for people with kidney problems. Rarely, long-term bisphosphonate therapy might cause pain and swelling in the jaw, vision problems or atypical hip fracture.
Prevention
Healthy lifestyle choices in early adulthood build a higher peak bone mass and reduce your risk of osteoporosis in later years. The same measures may lower your risk of falls and improve your overall health if you adopt them at any age.
To avoid falls and to maintain healthy bone:
- Get enough calcium and vitamin D. As a general rule, men and women age 50 and older should consume 1,200 milligrams of calcium a day, and 600 international units of vitamin D a day.
- Exercise to strengthen bones and improve balance. Weight-bearing exercises, such as walking, help you maintain peak bone density for more years. Exercise also increases your overall strength, making you less likely to fall. Balance training is also important to reducing your risk of falls, since balance tends to deteriorate with age.
- Avoid smoking or excessive drinking. Tobacco and alcohol use can reduce bone density. Drinking too much alcohol also can impair your balance and make you more likely to fall.
- Assess your home for hazards. Remove throw rugs, keep electrical cords against the wall, and clear excess furniture and anything else that could trip you. Make sure every room and passageway is well-lit.
- Check your eyes. Have an eye exam every other year, or more often if you have diabetes or an eye disease.
- Watch your medications. Feeling weak and dizzy, which are possible side effects of many medications, can increase your risk of falling. Talk to your doctor about side effects caused by your medications.
- Stand up slowly. Getting up too quickly can cause your blood pressure to drop and make you feel wobbly.
- Use a walking stick or walker. If you don’t feel steady when you walk, ask your doctor or occupational therapist whether these aids might help.