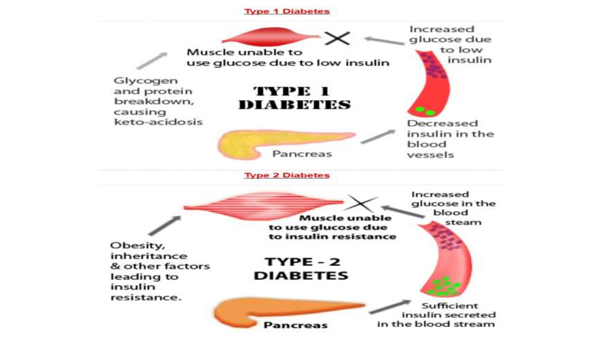
Type 2 diabetes
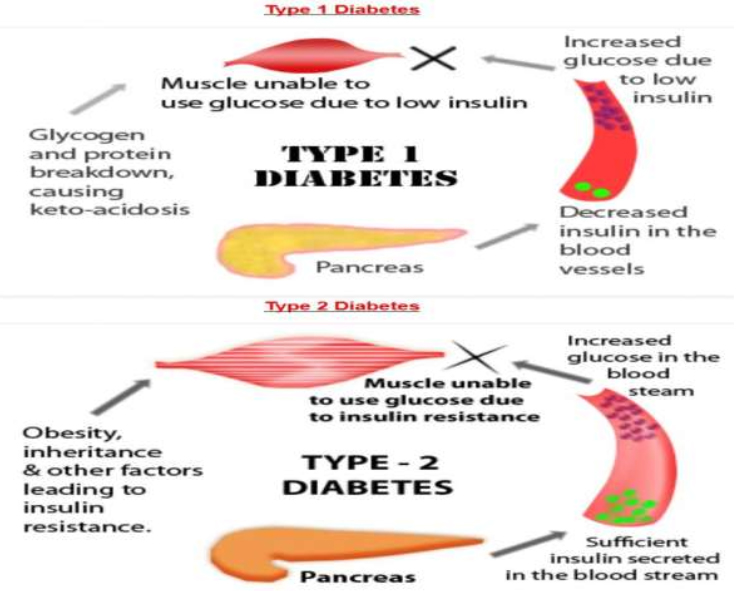
Type 2 diabetes, once known as adult-onset or noninsulin-dependent diabetes, is a chronic condition that affects the way your body metabolizes sugar (glucose), your body’s important source of fuel.
With type 2 diabetes, your body either resists the effects of insulin — a hormone that regulates the movement of sugar into your cells — or doesn’t produce enough insulin to maintain a normal glucose level.
More common in adults, type 2 diabetes increasingly affects children as childhood obesity increases. There’s no cure for type 2 diabetes, but you may be able to manage the condition by eating well, exercising and maintaining a healthy weight. If diet and exercise aren’t enough to manage your blood sugar well, you also may need diabetes medications or insulin therapy.
Symptoms
Type 2 diabetes symptoms often develop slowly. In fact, you can have type 2 diabetes for years and not know it. Look for:
- Increased thirst and frequent urination. Excess sugar building up in your bloodstream causes fluid to be pulled from the tissues. This may leave you thirsty. As a result, you may drink — and urinate — more than usual.
- Increased hunger. Without enough insulin to move sugar into your cells, your muscles and organs become depleted of energy. This triggers intense hunger.
- Weight loss. Despite eating more than usual to relieve hunger, you may lose weight. Without the ability to metabolize glucose, the body uses alternative fuels stored in muscle and fat. Calories are lost as excess glucose is released in the urine.
- Fatigue. If your cells are deprived of sugar, you may become tired and irritable.
- Blurred vision. If your blood sugar is too high, fluid may be pulled from the lenses of your eyes. This may affect your ability to focus.
- Slow-healing sores or frequent infections. Type 2 diabetes affects your ability to heal and resist infections.
- Areas of darkened skin. Some people with type 2 diabetes have patches of dark, velvety skin in the folds and creases of their bodies — usually in the armpits and neck. This condition, called acanthosis nigricans, may be a sign of insulin resistance.
Causes
Type 2 diabetes develops when the body becomes resistant to insulin or when the pancreas stops producing enough insulin. Exactly why this happens is unknown, although genetics and environmental factors, such as excess weight and inactivity, seem to be contributing factors.
How insulin works
Insulin is a hormone that comes from the gland situated behind and below the stomach (pancreas).
- The pancreas secretes insulin into the bloodstream.
- The insulin circulates, enabling sugar to enter your cells.
- Insulin lowers the amount of sugar in your bloodstream.
- As your blood sugar level drops, so does the secretion of insulin from your pancreas.
The role of glucose
Glucose — a sugar — is a main source of energy for the cells that make up muscles and other tissues.
- Glucose comes from two major sources: food and your liver.
- Sugar is absorbed into the bloodstream, where it enters cells with the help of insulin.
- Your liver stores and makes glucose.
- When your glucose levels are low, such as when you haven’t eaten in a while, the liver breaks down stored glycogen into glucose to keep your glucose level within a normal range.
In type 2 diabetes, this process doesn’t work well. Instead of moving into your cells, sugar builds up in your bloodstream. As blood sugar levels increase, the insulinproducing beta cells in the pancreas produce more insulin, but eventually these cells become impaired and can’t make enough insulin to meet the body’s demands.
In the much less common type 1 diabetes, the immune system destroys the beta cells, leaving the body with little to no insulin.
Treatments and drugs
Management of type 2 diabetes includes:
- Healthy eating
- Regular exercise
- Possibly, diabetes medication or insulin therapy
- Blood sugar monitoring
These steps will help keep your blood sugar level closer to normal, which can delay or prevent complications.
Healthy eating
Contrary to popular perception, there’s no specific diabetes diet. However, it’s important to center your diet on these high-fiber, low-fat foods:
- Fruits
- Vegetables
- Whole grains
You’ll also need to eat fewer animal products, refined carbohydrates and sweets.
Low glycemic index foods also may be helpful. The glycemic index is a measure of how quickly a food causes a rise in your blood sugar. Foods with a high glycemic index raise your blood sugar quickly. Low glycemic foods may help you achieve a more stable blood sugar. Foods with a low glycemic index typically are foods that are higher in fiber.
A registered dietitian can help you put together a meal plan that fits your health goals, food preferences and lifestyle. He or she can also teach you how to monitor your carbohydrate intake and let you know about how many carbohydrates you need to eat with your meals and snacks to keep your blood sugar levels more stable.
Physical activity
Everyone needs regular aerobic exercise, and people who have type 2 diabetes are no exception. Get your doctor’s OK before you start an exercise program. Then choose activities you enjoy, such as walking, swimming and biking. What’s most important is making physical activity part of your daily routine.
Aim for at least 30 minutes of aerobic exercise most days of the week. Stretching and strength training exercises are important, too. If you haven’t been active for a while, start slowly and build up gradually.
A combination of exercises — aerobic exercises, such as walking or dancing on most days, combined with resistance training, such as weightlifting or yoga twice a week — often helps control blood sugar more effectively than either type of exercise alone.
Remember that physical activity lowers blood sugar. Check your blood sugar level before any activity. You might need to eat a snack before exercising to help prevent low blood sugar if you take diabetes medications that lower your blood sugar.
Monitoring your blood sugar
Depending on your treatment plan, you may check and record your blood sugar level every now and then or, if you’re on insulin, multiple times a day. Ask your doctor how often he or she wants you to check your blood sugar. Careful monitoring is the only way to make sure that your blood sugar level remains within your target range.
Sometimes, blood sugar levels can be unpredictable. With help from your diabetes treatment team, you’ll learn how your blood sugar level changes in response to food, exercise, alcohol, illness and medication.
Diabetes medications and insulin therapy
Some people who have type 2 diabetes can achieve their target blood sugar levels with diet and exercise alone, but many also need diabetes medications or insulin therapy. The decision about which medications are best depends on many factors, including your blood sugar level and any other health problems you have. Your doctor might even combine drugs from different classes to help you control your blood sugar in several different ways.
Examples of possible treatments for type 2 diabetes include:
- Metformin (Glucophage, Glumetza, others). Generally, metformin is the first medication prescribed for type 2 diabetes. It works by improving the sensitivity of your body tissues to insulin so that your body uses insulin more effectively. Metformin also lowers glucose production in the liver. Metformin usually won’t lower blood sugar enough on its own. Your doctor will also recommend lifestyle changes, such as losing weight and becoming more active. Nausea and diarrhea are possible side effects of metformin. These side effects usually go away as your body gets used to the medicine. If metformin and lifestyles changes aren’t enough to control your blood sugar level, other oral or injected medications can be added.
- Sulfonylureas. These medications help your body secrete more insulin. Examples of medications in this class include glyburide (DiaBeta, Glynase), glipizide (Glucotrol) and glimepiride (Amaryl). Possible side effects include low blood sugar and weight gain.
- Meglitinides. These medications work like sulfonylureas by encouraging the body to secrete more insulin, but they’re faster acting, and they don’t stay active in the body for as long. They also have a risk of causing low blood sugar, but not as much risk as sulfonylureas do. Weight gain is a possibility with this class of medications as well. Examples include repaglinide (Prandin) and nateglinide (Starlix).
- Thiazolidinediones. Like metformin, these medications make the body’s tissues more sensitive to insulin. This class of medications has been linked to weight gain and other more serious side effects, such as an increased risk of heart failure and fractures. Because of these risks, these medications generally aren’t a first-choice treatment.Rosiglitazone (Avandia) and pioglitazone (Actos) are examples of thiazolidinediones
- DPP-4 inhibitors. These medications help reduce blood sugar levels, but tend to have a modest effect. They don’t seem to cause weight gain. Examples of these medications are sitagliptin (Januvia), saxagliptin (Onglyza) and linagliptin (Tradjenta).
- GLP-1 receptor agonists. These medications slow digestion and help lower blood sugar levels, though not as much as sulfonylureas. This class of medications isn’t recommended for use alone. Exenatide (Byetta) and liraglutide (Victoza) are examples of GLP-1 receptor agonists. Possible side effects include nausea and an increased risk of pancreatitis.
- SGLT2 inhibitors. These are the newest diabetes drugs on the market. They work by preventing the kidneys from reabsorbing sugar in the blood. Instead, the sugar is excreted in the urine. Examples include canagliflozin (Invokana) and dapagliflozin (Farxiga). Side effects may include yeast infections and urinary tract infections.
- Insulin therapy. Some people who have type 2 diabetes need insulin therapy as well. In the past, insulin therapy was used as last resort, but today it’s often prescribed sooner because of its benefits. Because normal digestion interferes with insulin taken by mouth, insulin must be injected. Depending on your needs, your doctor may prescribe a mixture of insulin types to use throughout the day and night. Often, people with type 2 diabetes start insulin use with one long-acting shot at night. Insulin injections involve using a fine needle and syringe or an insulin pen injector — a device that looks similar to an ink pen, except the cartridge is filled with
insulin.There are many types of insulin, and they each work in a different way. Options include:- Insulin glulisine (Apidra)
- Insulin lispr
- (Humalog)
- Insulin aspart (Novolog)
- Insulin glargine (Lantus)
- Insulin detemir (Levemir)
- Insulin isophane (Humulin N, Novolin N)
Discuss the pros and cons of different drugs with your doctor. Together you can decide which medication is best for you after considering many factors, including costs and other aspects of your health. In addition to diabetes medications, your doctor might prescribe low-dose aspirin therapy as well as blood pressure and cholesterol-lowering medications to help prevent heart and blood vessel disease.
Bariatric surgery
If you have type 2 diabetes and your body mass index (BMI) is greater than 35, you may be a candidate for weight-loss surgery (bariatric surgery). Blood sugar levels return to normal in 55 to 95 percent of people with diabetes, depending on the procedure performed. Surgeries that bypass a portion of the small intestine have more of an effect on blood sugar levels than do other weight-loss surgeries.
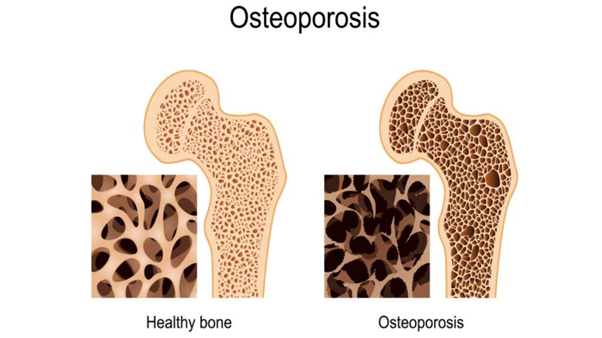
Drawbacks to the surgery include cost, and there are risks involved, including a risk of death. Additionally, drastic lifestyle changes are required and long-term complications may include nutritional deficiencies and osteoporosis.
Pregnancy
Women with type 2 diabetes may need to alter their treatment during pregnancy. Many women use insulin therapy during pregnancy. Cholesterol-lowering medications and some blood pressure drugs can’t be used during pregnancy.
If you have signs of diabetic retinopathy, it may worsen during pregnancy. Visit your ophthalmologist during the first trimester of your pregnancy and at one year postpartum.
Signs of trouble
Because so many factors can affect your blood sugar, problems sometimes arise that require immediate care, such as:
- High blood sugar (hyperglycemia). Your blood sugar level can rise for many reasons, including eating too much, being sick or not taking enough glucoselowering medication. Check your blood sugar level often, and watch for signs and symptoms of high blood sugar — frequent urination, increased thirst, dry mouth, blurred vision, fatigue and nausea. If you have hyperglycemia, you’ll need to adjust your meal plan, medications or both.
- Hyperglycemic hyperosmolar nonketotic syndrome (HHNS). Signs and symptoms of this life-threatening condition include a blood sugar reading higher than 600 mg/dL (33.3 mmol/L), dry mouth, extreme thirst, fever greater than 101 F (38 C), drowsiness, confusion, vision loss, hallucinations and dark urine. Your blood sugar monitor may not be able to give you an exact reading at such high levels and may instead just read “high.”HHNS is caused by sky-high blood sugar that turns blood thick and syrupy. It tends to be more common in older people with type 2 diabetes, and it’s often preceded by an illness or infection. HHNS usually develops over days or weeks. Call your doctor or seek immediate medical care if you have signs or symptoms of this condition.
- Increased ketones in your urine (diabetic ketoacidosis). If your cells are starved for energy, your body may begin to break down fat. This produces toxic acids known as ketones. Watch for loss of appetite, weakness, vomiting, fever, stomach pain and fruitysmelling breath. You can check your urine for excess ketones with an over-thecounter ketones test kit. If you have excess ketones in your urine, consult your doctor right away or seek emergency care. This condition is more common in people with type 1 diabetes but can sometimes occur in people with type 2 diabetes.
- Low blood sugar (hypoglycemia). If your blood sugar level drops below your target range, it’s known as low blood sugar (hypoglycemia). Your blood sugar level can drop for many reasons, including skipping a meal or getting more physical activity than normal. Low blood sugar is most likely if you take glucose-lowering medications that promote the secretion of insulin or if you’re taking insulin.Check your blood sugar level regularly, and watch for signs and symptoms of low blood sugar — sweating, shakiness, weakness, hunger, dizziness, headache, blurred vision, heart palpitations, slurred speech, drowsiness, confusion and seizures.If you develop hypoglycemia during the night, you might wake with sweat-soaked pajamas or a headache. Due to a natural rebound effect, nighttime hypoglycemia might cause an unusually high blood sugar reading first thing in the morning.
If you have signs or symptoms of low blood sugar, drink or eat something that will quickly raise your blood sugar level — fruit juice, glucose tablets, hard candy, regular (not diet) soda or another source of sugar. Retest in 15 minutes to be sure your blood glucose levels are normal.
If they’re not, treat again and retest in another 15 minutes. If you lose consciousness, a family member or close contact may need to give you an emergency injection of a hormone that stimulates the release of sugar into the blood (glucagon).
Prevention
Healthy lifestyle choices can help you prevent type 2 diabetes. Even if you have diabetes in your family, diet and exercise can help you prevent the disease. If you’ve already received a diagnosis of diabetes, you can use healthy lifestyle choices to help prevent complications. And if you have prediabetes, lifestyle changes can slow or halt the progression from prediabetes to diabetes.
- Eat healthy foods. Choose foods lower in fat and calories and higher in fiber. Focus on fruits, vegetables and whole grains.
- Get physical. Aim for 30 minutes of moderate physical activity a day. Take a brisk daily walk. Ride a bike. Swim laps. If you can’t fit in a long workout, spread 10- minute or longer sessions throughout the day.
- Lose excess pounds. If you’re overweight, losing 7 percent of your body weight can reduce the risk of diabetes. To keep your weight in a healthy range, focus on permanent changes to your eating and exercise habits. Motivate yourself by remembering the benefits of losing weight, such as a healthier heart, more energy and improved self-esteem.
Sometimes medication is an option as well. Metformin (Glucophage, Glumetza, others), an oral diabetes medication, may reduce the risk of type 2 diabetes — but healthy lifestyle choices remain essential.