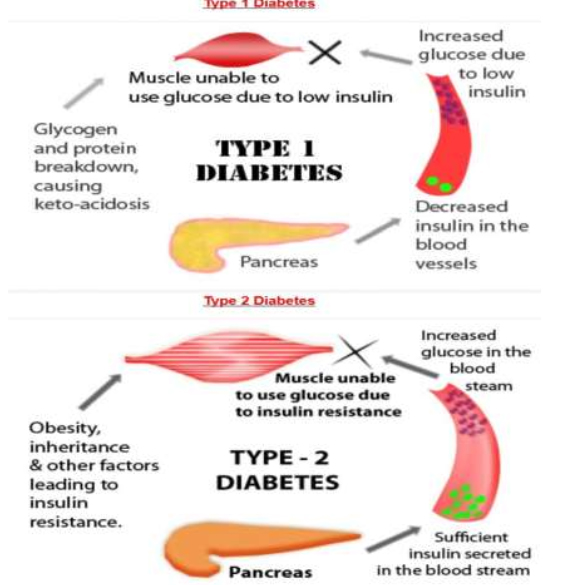
Diabetes mellitus refers to a group of diseases that affect how your body uses blood sugar (glucose). Glucose is vital to your health because it’s an important source of energy for the cells that make up your muscles and tissues. It’s also your brain’s main source of fuel.
If you have diabetes, no matter what type, it means you have too much glucose in your blood, although the causes may differ. Too much glucose can lead to serious health problems.
Chronic diabetes conditions include type 1 diabetes and type 2 diabetes. Potentially reversible diabetes conditions include prediabetes — when your blood sugar levels are higher than normal, but not high enough to be classified as diabetes — and gestational diabetes, which occurs during pregnancy but may resolve after the baby is delivered.
Symptoms
Diabetes symptoms vary depending on how much your blood sugar is elevated. Some people, especially those with prediabetes or type 2 diabetes, may not experience symptoms initially. In type 1 diabetes, symptoms tend to come on quickly and be more severe.
Some of the signs and symptoms of type 1 and type 2 diabetes are:
- Increased thirst
- Frequent urination
- Extreme hunger
- Unexplained weight loss
- Presence of ketones in the urine (ketones are a byproduct of the breakdown of muscle and fat that happens when there’s not enough available insulin)
- Fatigue
- Irritability
- Blurred vision
- Slow-healing sores
- Frequent infections, such as gums or skin infections and vaginal infections
Although type 1 diabetes can develop at any age, it typically appears during childhood or adolescence. Type 2 diabetes, the more common type, can develop at any age, though it’s more common in people older than 40.
Causes
To understand diabetes, first you must understand how glucose is normally processed in the body.
How insulin works
Insulin is a hormone that comes from a gland situated behind and below the stomach (pancreas).
- The pancreas secretes insulin into the bloodstream.
- The insulin circulates, enabling sugar to enter your cells.
- Insulin lowers the amount of sugar in your bloodstream.
- As your blood sugar level drops, so does the secretion of insulin from your pancreas
The role of glucose
Glucose — a sugar — is a source of energy for the cells that make up muscles and other tissues.
- Glucose comes from two major sources: food and your liver.
- Sugar is absorbed into the bloodstream, where it enters cells with the help of insulin.
- Your liver stores and makes glucose.
- When your glucose levels are low, such as when you haven’t eaten in a while, the liver breaks down stored glycogen into glucose to keep your glucose level within a normal range.
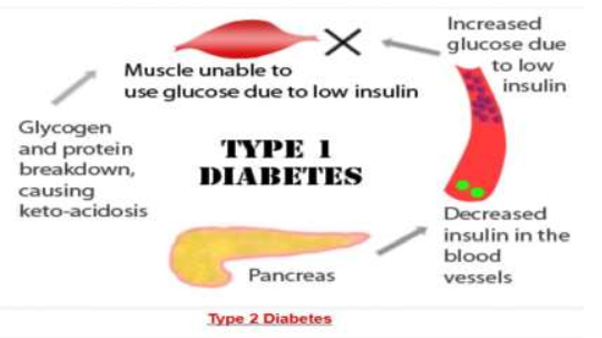
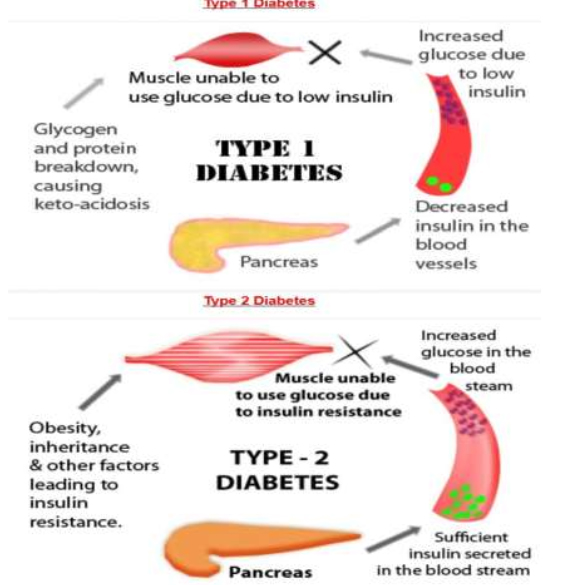
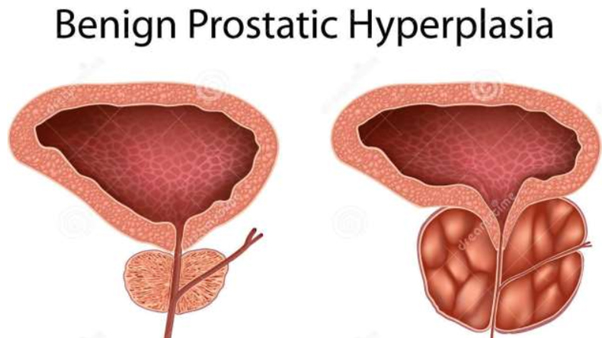
Causes of type 1 diabetes
The exact cause of type 1 diabetes is unknown. What is known is that your immune system — which normally fights harmful bacteria or viruses — attacks and destroys your insulin-producing cells in the pancreas. This leaves you with little or no insulin. Instead of being transported into your cells, sugar builds up in your bloodstream.
Type 1 is thought to be caused by a combination of genetic susceptibility and environmental factors, though exactly what many of those factors are is still unclear.
Causes of prediabetes and type 2 diabetes
In prediabetes — which can lead to type 2 diabetes — and in type 2 diabetes, your cells become resistant to the action of insulin, and your pancreas is unable to make enough insulin to overcome this resistance. Instead of moving into your cells where it’s needed for energy, sugar builds up in your bloodstream.
Exactly why this happens is uncertain, although it’s believed that genetic and environmental factors play a role in the development of type 2 diabetes. Being overweight is strongly linked to the development of type 2 diabetes, but not everyone with type 2 is overweight.
Causes of gestational diabetes
During pregnancy, the placenta produces hormones to sustain your pregnancy. These hormones make your cells more resistant to insulin.
Normally, your pancreas responds by producing enough extra insulin to overcome this resistance. But sometimes your pancreas can’t keep up. When this happens, too little glucose gets into your cells and too much stays in your blood, resulting in gestational diabetes.
Treatments and drugs
Depending on what type of diabetes you have, blood sugar monitoring, insulin and oral medications may play a role in your treatment. Eating a healthy diet, maintaining a healthy weight and participating in regular activity also are important factors in managing diabetes.
Treatments for all types of diabetes
An important part of managing diabetes — as well as your overall health — is maintaining a healthy weight through a healthy diet and exercise plan:
- Healthy eating. Contrary to popular perception, there’s no specific diabetes diet. You’ll need to center your diet on more fruits, vegetables and whole grains — foods that are high in nutrition and fiber and low in fat and calories — and cut down on animal products, refined carbohydrates and sweets. In fact, it’s the best eating plan for the entire family. Sugary foods are OK once in a while, as long as they’re counted as part of your meal plan.Yet understanding what and how much to eat can be a challenge. A registered dietitian can help you create a meal plan that fits your health goals, food preferences and lifestyle. This will likely include carbohydrate counting, especially if you have type 1 diabetes.
- Physical activity. Everyone needs regular aerobic exercise, and people who have diabetes are no exception. Exercise lowers your blood sugar level by moving sugar into your cells, where it’s used for energy. Exercise also increases your sensitivity to insulin, which means your body needs less insulin to transport sugar to your cells. Get your doctor’s OK to exercise. Then choose activities you enjoy, such as walking, swimming or biking. What’s most important is making physical activity part of your daily routine. Aim for at least 30 minutes or more of aerobic exercise most days of the week. If you haven’t been active for a while, start slowly and build up gradually.
Treatments for type 1 and type 2 diabetes
Treatment for type 1 diabetes involves insulin injections or the use of an insulin pump, frequent blood sugar checks, and carbohydrate counting. Treatment of type 2 diabetes primarily involves monitoring of your blood sugar, along with diabetes medications, insulin or both.
- Monitoring your blood sugar. Depending on your treatment plan, you may check and record your blood sugar as often as several times a week to as many as four to eight times a day. Careful monitoring is the only way to make sure that your blood sugar level remains within your target range. People who receive insulin therapy also may choose to monitor their blood sugar levels with a continuous glucose monitor. Although this technology doesn’t yet replace the glucose meter, it can provide important information about trends in blood sugar levels.Even with careful management, blood sugar levels can sometimes change unpredictably. With help from your diabetes treatment team, you’ll learn how your blood sugar level changes in response to food, physical activity, medications, illness, alcohol, stress — for women, fluctuations in hormone levels.In addition to daily blood sugar monitoring, your doctor will likely recommend regular A1C testing to measure your average blood sugar level for the past two to three months. Compared with repeated daily blood sugar tests, A1C testing better indicates how well your diabetes treatment plan is working overall. An elevated A1C level may signal the need for a change in your insulin regimen or meal plan. Your target A1C goal may vary depending on your age and various other factors. However, for most people with diabetes, the American Diabetes Association recommends an A1C of below 7 percent. Ask your doctor what your A1C target is.
- Insulin. People with type 1 diabetes need insulin therapy to survive. Many people with type 2 diabetes or gestational diabetes also need insulin therapy.Many types of insulin are available, including rapid-acting insulin, long-acting insulin and intermediate options. Depending on your needs, your doctor may prescribe a mixture of insulin types to use throughout the day and night.Insulin can’t be taken orally to lower blood sugar because stomach enzymes interfere with insulin’s action. Often insulin is injected using a fine needle and syringe or an insulin pen — a device that looks like a large ink pen.An insulin pump may also be an option. The pump is a device about the size of a cellphone worn on the outside of your body. A tube connects the reservoir of insulin to a catheter that’s inserted under the skin of your abdomen. A tubeless pump that works wirelessly is also now available. You program an insulin pump to dispense specific amounts of insulin. It can be adjusted to deliver more or less insulin depending on meals, activity level and blood sugar level.
An emerging treatment approach, not yet available, is closed loop insulin delivery, also known as the artificial pancreas. It links a continuous glucose monitor to an insulin pump. The device automatically delivers the correct amount of insulin when the monitor indicates the need for it. There are a number of different versions of the artificial pancreas, and clinical trials have had encouraging results. More research needs to be done before a fully functional artificial pancreas can receive regulatory approval.
However, the first step toward an artificial pancreas was approved in 2013. Combining a continuous glucose monitor with an insulin pump, this system stops insulin delivery when blood sugar levels drop too low. Studies on the device found that it could prevent low blood sugar levels overnight without significantly increasing morning blood sugar levels.
- Oral or other medications. Sometimes other oral or injected medications are prescribed as well. Some diabetes medications stimulate your pancreas to produce and release more insulin. Others inhibit the production and release of glucose from your liver, which means you need less insulin to transport sugar into your cells. Still others block the action of stomach or intestinal enzymes that break down carbohydrates or make your tissues more sensitive to insulin. Metformin (Glucophage, Glumetza, others) is generally the first medication prescribed for type 2 diabetes.
- Transplantation. In some people who have type 1 diabetes, a pancreas transplant may be an option. Islet transplants are being studied as well. With a successful pancreas transplant, you would no longer need insulin therapy. But transplants aren’t always successful — and these procedures pose serious risks. You need a lifetime of immune-suppressing drugs to prevent organ rejection. These drugs can have serious side effects, including a high risk of infection, organ injury and cancer. Because the side effects can be more dangerous than the diabetes, transplants are usually reserved for people whose diabetes can’t be controlled or those who also need a kidney transplant.
- Bariatric surgery. Although it is not specifically considered a treatment for type 2 diabetes, people with type 2 diabetes who also have a body mass index higher than 35 may benefit from this type of surgery. People who’ve undergone gastric bypass have seen significant improvements in their blood sugar levels. However, this procedure’s long-term risks and benefits for type 2 diabetes aren’t yet known.
Treatment for gestational diabetes
Controlling your blood sugar level is essential to keeping your baby healthy and avoiding complications during delivery. In addition to maintaining a healthy diet and exercising, your treatment plan may include monitoring your blood sugar and, in some cases, using insulin or oral medications.
Your health care provider will also monitor your blood sugar level during labor. If your blood sugar rises, your baby may release high levels of insulin — which can lead to low blood sugar right after birth.
Treatment for prediabetes
If you have prediabetes, healthy lifestyle choices can help you bring your blood sugar level back to normal or at least keep it from rising toward the levels seen in type 2 diabetes. Maintaining a healthy weight through exercise and healthy eating can help. Exercising at least 150 minutes a week and losing 5 to 10 percent of your body weight may prevent or delay type 2 diabetes.
Sometimes medications — such as metformin (Glucophage, Glumetza, others) — also are an option if you’re at high risk of diabetes, including when your prediabetes is worsening or if you have cardiovascular disease, fatty liver disease or polycystic ovary syndrome.
In other cases, medications to control cholesterol — statins, in particular — and high blood pressure medications are needed. Your doctor might prescribe low-dose aspirin therapy to help prevent cardiovascular disease if you’re at high risk. Healthy lifestyle choices remain key, however.
Signs of trouble in any type of diabetes
Because so many factors can affect your blood sugar, problems may sometimes arise that require immediate care, such as:
- High blood sugar (hyperglycemia). Your blood sugar level can rise for many reasons, including eating too much, being sick or not taking enough glucoselowering medication. Check your blood sugar level as directed by your doctor, and watch for signs and symptoms of high blood sugar — frequent urination, increased thirst, dry mouth, blurred vision, fatigue and nausea. If you have hyperglycemia, you’ll need to adjust your meal plan, medications or both.
- Increased ketones in your urine (diabetic ketoacidosis). If your cells are starved for energy, your body may begin to break down fat. This produces toxic acids known as ketones. Watch for loss of appetite, weakness, vomiting, fever, stomach pain and a sweet, fruity breath. You can check your urine for excess ketones with an over-thecounter ketones test kit. If you have excess ketones in your urine, consult your doctor right away or seek emergency care. This condition is more common in people with type 1 diabetes.
- Hyperglycemic hyperosmolar nonketotic syndrome. Signs and symptoms of this life-threatening condition include a blood sugar reading over 600 mg/dL (33.3 mmol/L), dry mouth, extreme thirst, fever, drowsiness, confusion, vision loss and hallucinations. Hyperosmolar syndrome is caused by sky-high blood sugar that turns blood thick and syrupy. It tends to be more common in people with type 2 diabetes, and it’s often preceded by an illness. Call your doctor or seek immediate medical care if you have signs or symptoms of this condition.
- Low blood sugar (hypoglycemia). If your blood sugar level drops below your target range, it’s known as low blood sugar (hypoglycemia). Your blood sugar level can drop for many reasons, including skipping a meal and getting more physical activity than normal. However, low blood sugar is most likely if you take glucoselowering medications that promote the secretion of insulin by your pancreas or if you’re receiving insulin therapy. Check your blood sugar level regularly, and watch for signs and symptoms of low blood sugar — sweating, shakiness, weakness, hunger, dizziness, headache, blurred vision, heart palpitations, irritability, slurred speech, drowsiness, confusion, fainting and seizures. Low blood sugar is treated with quickly absorbed carbohydrates, such as fruit juice or glucose tablets.
Prevention
Type 1 diabetes can’t be prevented. However, the same healthy lifestyle choices that help treat prediabetes, type 2 diabetes and gestational diabetes can also help prevent them:
- Eat healthy foods. Choose foods lower in fat and calories and higher in fiber. Focus on fruits, vegetables and whole grains. Strive for variety to prevent boredom.
- Get more physical activity. Aim for 30 minutes of moderate physical activity a day. Take a brisk daily walk. Ride your bike. Swim laps. If you can’t fit in a long workout, break it up into smaller sessions spread throughout the day.
- Lose excess pounds. If you’re overweight, losing even 7 percent of your body weight — for example, 14 pounds (6.4 kilograms) if you weigh 200 pounds (90.9 kilograms) — can reduce the risk of diabetes. To keep your weight in a healthy range, focus on permanent changes to your eating and exercise habits. Motivate yourself by remembering the benefits of losing weight, such as a healthier heart, more energy and improved self-esteem.
- Sometimes medication is an option as well. Oral diabetes drugs such as metformin (Glucophage, Glumetza, others) may reduce the risk of type 2 diabetes — but healthy lifestyle choices remain essential.
- Have your blood sugar checked at least once a year to check that you haven’t developed type 2 diabetes.